Dry Eye Disease
Dry Eye Disease is a largely underdiagnosed condition that occurs when the eyes do not make enough tears or the tears evaporate too quickly. It’s generally not sight-threatening but if left untreated, the symptoms – itching, discomfort, and irritation – become worse and can increase the risk of infection and other visual problems. It is important for patients with this condition to take special care of their eyes in order to alleviate symptoms and prevent complications. The diagnosis of Dry Eye is often missed because allergy, eyestrain, and fatigue have similar symptoms. Your Eye doctor will determine if you have dry eyes, and provide a customized treatment tailored specifically for you. It is important that Dry Eye is managed correctly in order to prevent possible associated infections and/or visual disturbances that can occur if left untreated. Your doctor can diagnose dry eye after a thorough evaluation of your eyes and tear production with a Schirmer tear test and Tearlab Osmolarity testing.
Understanding your Tear Film
Our eyes need a constant layer of tears – called the tear film – to maintain and protect the sensitive surface tissues. Dry eye syndrome occurs when there is a lack of adequate tears. For some people, the cause of dry eyes is an imbalance in the composition of their tears. Other people don’t produce enough tears to keep their eyes comfortably lubricated.
Tears are Comprised of Three Layers
1) Lipid (oil) layer: Outermost Layer which lubricates the eyes and helps prevent tears from evaporating when the eyes are open.
2) Aqueous (water) layer: Middle Layer that is composed of water and nutrients that lubricate and nourish the cornea.
3) Mucin layer: Innermost Layer that coats the surface of the cornea and makes the tears adhere to, and spread evenly over the surface.
Changes or disruption to any one or more of the three tear film layers may interfere with the process of routine lubrication of the eye surface, resulting in Dry Eye Disease.
What should I do if I have Dry Eye symptoms?
Only a doctor can determine if you have Dry Eye Disease – and our doctors offer enhanced testing to provide an important diagnostic and predictive value. Test results are used to design a treatment approach tailored to your specific condition.
- A COMPREHENSIVE eye exam
- Measurement of the VOLUME of your tears
- Assessment of the QUALITY of your tears
- Tear Analysis measuring your TEAR OSMOLARITY
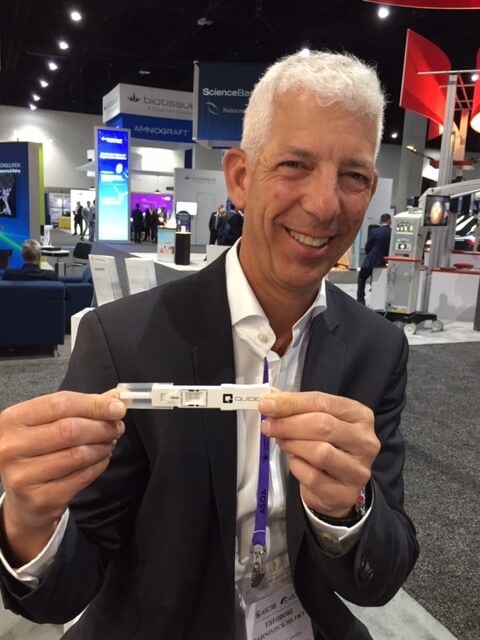
TEAR ANALYSIS
 We provide the latest tear analyzer that tests TEAR OSMOLARITY. This non-invasive test determines the salt and enzyme concentration of your tear film. In fact, some doctors refer to it as the “thermometer of the eye” as it reflects the inflammation caused by elevated salt content.
We provide the latest tear analyzer that tests TEAR OSMOLARITY. This non-invasive test determines the salt and enzyme concentration of your tear film. In fact, some doctors refer to it as the “thermometer of the eye” as it reflects the inflammation caused by elevated salt content.
The American Academy of Ophthalmology (AAO) Preferred Practice Pattern for Dry Eye Syndrome specifically recommends tear osmolarity testing for the diagnosis and management of dry eye syndrome. Note that the TearLab tear osmolarity test is identified as “a more sensitive method of diagnosing and grading the severity of dry eye compared to corneal and conjunctival staining, tear break-up time, Schirmer test and meibomian gland grading”.
 Although not covered by Ontario Health Insurance Plan, it provides an important predictive value in determining the severity of an individual’s dry eye, and a meaningful measure of the health and stability of the protective tear film that covers the surface of your eyes.
Although not covered by Ontario Health Insurance Plan, it provides an important predictive value in determining the severity of an individual’s dry eye, and a meaningful measure of the health and stability of the protective tear film that covers the surface of your eyes.
Why Do Eyes Become Dry?
There are two main reasons why eyes become dry:
Aqueous Deficient Dry Eye (DED)
Aqueous Deficient Dry Eye occurs when the tear secretion by the lacrimal glands is insufficient to maintain a healthy ocular surface. Aqueous Deficient Dry Eye is a chronic inflammation of the ocular surgace and has increasingly strong ties to autoimmune diseases such as diabetes, thyroid disease, and rheumatoid arthritis. This condition is significantly more prevalen in women and only represents about 15% of all dry eye patients.
Evaporative Dry Eye (MGD)
Evaporative Dry Eye (MGD) occurs when the outer lipid layer of the normal tear film is deficient and as a result, the tear film evaporates too quickly. This often occurs when the meibomian glands in the eyelids are inflamed or damaged (Meibomian Gland Dysfunction), such as blepharitis. Evaporative Dry Eye conditions make up 85% of the dry eye population.
Patients can suffer a mixed mechanism of both Aqueous Deficient and Evaporative Dry Eye.
In some instances, dry eye can be related to other conditions and their treatment. For example, a link has been found between dry eye, sleep apnea, and the use of a CPAP. For information regarding dry eye and sleep apnea, visit one of the below links:
http://www.sleepreviewmag.com/2016/09/identifying-treating-dry-eye-obstructive-sleep-apnea-patients/
https://www.aoa.org/news/clinical-eye-care/sleep-apneas-effect-on-the-eyes
Diagnostic testing will determine the type of Dry Eye that you have and will help us to further develop a Personalized Treatment Plan.
Diagnostic Testing
Tear Lab or Osmolarity Testing
High tear osmolarity is the hallmark of dry eye disease. This test involves taking a direct sample of your tears to measure the saltiness and overall composition. This test provides a numerical value of osmolarity to allow for grading of severity and to monitor the effectiveness of treatment. Patients with dry eye will have an osmolarity higher than 308 mOsm/L and/or a difference between the eyesof greater than 8 mOsm/L.
Lipiscan
This diagnostic test allows us to get an image of the meibomian glands located within the eyelids. These glands secrete meibum (oil) which is a significant component of the tear film. Decreased meibum production leads to evaporation of tears from the eye. Patients who have dysfunctional glands can have shortening or complete loss of glands, which is visible with this imaging.
HD Analyzer
This technology provides us with an objective and non-invasive analysis of how the tear film is behaving over a 20 second interval, allowing us to evaluate how successful a patient’s blink is at restoring tear function.
Inflammadry
This is a direct measure for the presence of inflammation on the ocular surface by detecting the level of matrix metallipeptidase 9, an inflammatory marker that is consistently elevated in the tears of patients with dry eye.